7 Key Differences in Holistic vs Traditional Health Care

Disclosure: The information provided is for educational purposes only and not intended as medical advice. Consult a healthcare professional before making any changes to your health routine. If you make a purchase through the links provided, I may earn a small commission at no additional cost to you.
Are you trapped in a cycle of treating symptoms, only to watch the same issues resurface over and over again? Choosing between holistic and traditional health care isn’t just about preference—it’s about understanding how these two approaches shape your health journey. Traditional care focuses on treating symptoms and managing conditions, often with medication or surgery.
Holistic care, on the other hand, aims to address root causes, treating the body, mind, and spirit as interconnected. In this article, we’ll explore seven key differences that highlight how these systems approach wellness, prevention, and patient care, helping you choose the path that aligns with your goals.
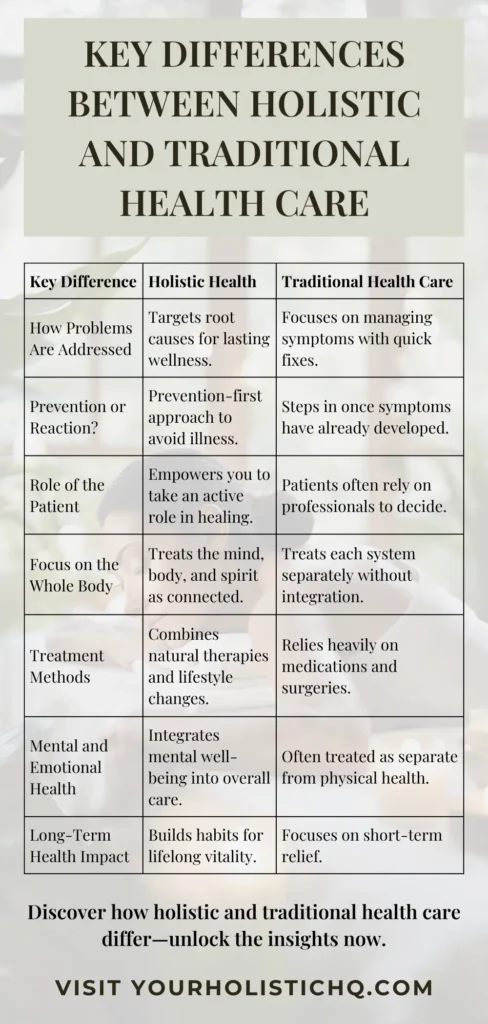
1. Focus on Root Causes vs. Symptoms

Traditional health care often targets symptoms to provide immediate relief, a necessary approach in acute or emergency situations. For instance, a person experiencing chronic back pain might receive painkillers or anti-inflammatory drugs to manage their discomfort. While effective in the short term, these solutions often fail to address the root cause—such as poor posture, muscle imbalances, or stress—leading to recurring or worsening issues. This symptom-focused strategy, while crucial in certain scenarios, can leave underlying problems unaddressed.
Holistic health care, by contrast, prioritizes identifying and resolving the root causes of health concerns. For example, a holistic practitioner addressing chronic back pain might assess the patient’s lifestyle, including work ergonomics, stress levels, and physical activity. Treatment could involve a combination of physical therapy, mindfulness practices to reduce stress, and exercises to strengthen supporting muscles. This multifaceted approach not only alleviates pain but also addresses the conditions that caused it, reducing the likelihood of recurrence.
Research highlights the effectiveness of focusing on root causes. A study in The Lancet demonstrated that lifestyle changes like improved nutrition, regular exercise, and stress management reduced the risk of chronic conditions such as heart disease by up to 72%. Similarly, findings from the Journal of Preventive Medicine revealed that patients addressing stress and dietary imbalances significantly lowered their chances of developing type 2 diabetes. These examples illustrate how treating root causes can lead to long-term health improvements, rather than temporary symptom relief.
2. Integration of Care

In traditional health care, primary care physicians often serve as the initial point of contact for patients, providing assessments, basic treatments, and referrals to specialists when needed. This “gatekeeping” role is designed to streamline care, ensuring that patients access the appropriate expertise for complex or specialized conditions. For instance, a patient experiencing chest pain might visit their primary care physician, who would perform initial tests, such as blood pressure measurements or an electrocardiogram (ECG). If a cardiac issue is suspected, the PCP would refer the patient to a cardiologist for further evaluation. This process is intended to prevent misdiagnosis and ensure that serious conditions receive timely attention.
However, this system can sometimes lead to inefficiencies and higher costs. If the PCP refers a patient as a precautionary measure, even when the issue could be addressed at the primary care level, the patient may end up paying for multiple consultations and tests. For example, chest pain caused by musculoskeletal strain or stress might require lifestyle advice, physical therapy, or stress-management techniques—interventions that a PCP could provide. Yet, due to liability concerns, time constraints, or limited access to resources, they may instead refer the patient to a cardiologist, leading to additional expenses and fragmented care.
Holistic health care seeks to address such gaps by offering more integrated and comprehensive evaluations in a single setting. Practitioners consider the patient’s physical, emotional, and lifestyle factors, addressing interconnected causes rather than focusing solely on specific symptoms. In the case of chest pain, a holistic approach might involve identifying stress as a trigger, recommending relaxation techniques, and addressing posture or dietary habits to alleviate the issue. Research published in The Lancet highlights that holistic models, which prioritize integration, can reduce unnecessary referrals and associated costs, while improving patient outcomes through a more cohesive approach to care.
3. Proactive Prevention

Traditional health care often steps in after symptoms or conditions have fully developed, addressing problems only when they’ve reached a critical stage. For instance, a patient diagnosed with prediabetes may be prescribed medications to manage blood sugar levels, but without addressing the underlying cause: insulin resistance. This condition silently develops as cells become less responsive to insulin, forcing the body to compensate by producing more. Left untreated, insulin resistance can lead to a cascade of health issues, including diabetes, heart disease, and even cognitive decline.
Holistic health care takes a different approach, focusing on early intervention to prevent such conditions before they become chronic. Practitioners address contributing factors like poor diet, inactivity, and stress through targeted strategies such as ancestral nutrition, which emphasizes whole, nutrient-dense foods that align with how humans are biologically designed to eat. For example, prioritizing grass-fed meats, fermented foods, and healthy fats can stabilize blood sugar and reduce inflammation. This, paired with stress-reduction techniques and regular resistance training, not only mitigates risk factors but also builds resilience against future health challenges.
The urgency of prevention is backed by research. A study in Diabetes Care revealed that 90% of individuals with prediabetes were unaware of their condition despite showing clear signs of insulin resistance. Another study in The Lancet demonstrated that lifestyle interventions, including ancestral nutrition and consistent physical activity, could reverse insulin resistance within six months, significantly reducing the progression to diabetes. Such findings highlight the critical role of proactive, holistic strategies in achieving long-term health.
4. Active Patient Involvement

In traditional health care, patients often follow a passive model, relying on doctors to diagnose and treat health conditions without fully understanding their role in the process. For instance, a person managing type 2 diabetes might adhere to a medication regimen but remain unaware of how dietary choices, stress, and physical activity influence their disease. This approach can leave patients feeling disengaged and dependent on external solutions.
Holistic health care flips this dynamic by placing patients at the center of their wellness journey. Practitioners actively collaborate with individuals to create personalized plans that account for their lifestyle, preferences, and goals. For example, a patient managing type 2 diabetes might work with a holistic practitioner to co-create a plan involving nutrient-dense meals, stress management tools, and regular movement tailored to their abilities. This approach empowers patients to make informed decisions and take responsibility for their health.
Research underscores the effectiveness of patient involvement. A study published in The BMJ showed that individuals who participated in setting health goals and tracking their progress experienced a 35% improvement in outcomes compared to those following standard care. These findings demonstrate the power of holistic care’s emphasis on education, collaboration, and self-empowerment in achieving sustainable health outcomes.
5. Diverse Treatment Methods

Traditional health care predominantly relies on medications and surgical interventions to manage health conditions. For example, a patient with chronic joint pain might receive prescription pain relievers or cortisone injections. While these treatments can provide immediate relief, they often address symptoms without resolving underlying issues, and long-term use may lead to side effects or complications.
Holistic health care employs a diverse range of treatment methods, blending conventional medicine with natural therapies. For chronic joint pain, a holistic practitioner might recommend a combination of acupuncture, anti-inflammatory dietary adjustments, gentle yoga, and stress-reduction practices. These integrative methods aim to alleviate pain while addressing contributing factors such as inflammation, stress, or posture imbalances, promoting overall healing and resilience.
Research supports the effectiveness of combining natural and conventional approaches. A study in The Journal of Alternative and Complementary Medicine found that acupuncture, when used alongside standard pain management therapies, reduced chronic pain intensity by 40% compared to conventional treatments alone. This evidence highlights the potential of holistic care to enhance treatment outcomes while minimizing reliance on medication.
6. Mental and Emotional Health Support

Traditional health care often separates mental and emotional health from physical health, addressing them through distinct specialties like psychiatry or psychology. For example, a patient suffering from anxiety might be prescribed medication or therapy to manage symptoms, but physical health factors—such as gut health, sleep quality, or nutritional deficiencies—are often overlooked. This segmented approach can leave underlying causes unaddressed, potentially limiting the effectiveness of treatment.
Holistic health care recognizes the interconnectedness of mental, emotional, and physical well-being, with a growing understanding that your gut microbiome impacts mental health. The gut-brain axis reveals how gut microbiota—trillions of bacteria in the gastrointestinal system—are key players in producing neurotransmitters like serotonin, which influences mood and emotional regulation. Disruptions in gut health, such as dysbiosis (an imbalance in gut bacteria), have been directly linked to anxiety and depression. A holistic approach to anxiety might include dietary changes to promote a healthy microbiome, such as increasing fiber intake or consuming fermented foods rich in probiotics. These interventions, combined with mindfulness practices and physical activity, address both symptoms and their root causes.
Research underscores the profound connection between gut health and mental well-being. A study in Nature Microbiology found that individuals with diverse gut microbiota reported lower levels of stress and anxiety. Similarly, a clinical trial in General Psychiatry demonstrated that probiotics significantly improved symptoms of depression by restoring gut balance. These findings highlight how addressing gut health as part of a holistic care plan offers a more comprehensive and effective path to mental wellness, integrating physical and emotional health for lasting results.
7. Personalized Care Plans

Traditional health care often relies on standardized treatment protocols designed for the general population. For instance, patients with hypertension might be prescribed the same class of medications regardless of individual lifestyle, genetics, or specific triggers. While effective in addressing common symptoms, this one-size-fits-all approach may overlook unique factors that influence each person’s health.
Holistic health care prioritizes personalization, tailoring treatment plans to the individual’s specific needs, preferences, and circumstances. A holistic practitioner addressing hypertension might incorporate a combination of natural therapies, such as stress-reduction techniques, dietary modifications, and herbal supplements, alongside conventional treatments. By considering factors like the patient’s daily habits, genetic predispositions, and emotional health, the approach creates a customized path to wellness.
Research supports the efficacy of personalized care. A study published in Nature Medicine demonstrated that individualized health plans, which integrate lifestyle, genetic, and environmental factors, improved patient outcomes by 45% compared to standardized treatments. This evidence highlights the strength of holistic care in delivering effective, patient-centered solutions.
Final Thoughts

Holistic health care provides a refreshing alternative to the symptom-focused nature of traditional health care. By addressing the root causes of health issues, integrating mental, physical, and emotional well-being, and encouraging active patient participation, it lays the foundation for long-term vitality. This comprehensive approach empowers individuals to take control of their health through sustainable lifestyle changes and personalized care.
While traditional health care remains indispensable for acute and emergency situations, combining it with holistic principles creates a more balanced and effective model. The integration of these two approaches allows for immediate solutions when needed while fostering preventive care and overall well-being in the long term.
Choosing between holistic and traditional health care doesn’t have to be an either-or decision. For many, the most effective path lies in blending the strengths of both systems. Exploring holistic health practices offers an opportunity to embrace a more comprehensive, interconnected perspective that enhances both health and quality of life.





