Vagus Nerve Symptoms: How One Nerve Links Your Gut, Heart & Mood
There’s a single nerve connecting your brain to nearly every major organ in your body—and chances are, no one’s ever talked to you about it.
It’s called the vagus nerve, and it plays a central role in regulating your digestion, heart rate, breathing, immune response, inflammation, and even your ability to feel calm, connected, or safe.
When this nerve gets disrupted—which happens very easily—it can affect everything from gut health to mood stability to energy levels.
Modern medicine tends to treat these symptoms in isolation. But your body doesn’t work in silos—and the vagus nerve proves it.
Ignore it, and you’ll keep chasing symptoms. Understand it, and the whole system starts to click.
- Vagus Nerve Symptoms: How One Nerve Links Your Gut, Heart & Mood
- 🔑 Quick Summary
- What Is the Vagus Nerve—And Why It Matters More Than You Think?
- What Happens When the Vagus Nerve Breaks Down—And Why Doctors Miss It
- What Causes Vagus Nerve Dysfunction?
- How to Recognize Vagus Nerve Dysfunction—Even When Doctors Don’t
- How to Support Vagus Nerve Function Naturally
- Why Your Doctor May Not Mention the Vagus Nerve
- Final Thoughts: Why the Vagus Nerve Deserves Your Attention
- ❓ FAQs
🔑 Quick Summary
— The vagus nerve links your brain to your gut, heart, lungs, and mood — and it’s the missing link in chronic symptoms
— Symptoms like anxiety, IBS, fatigue, and inflammation often trace back to vagus nerve dysfunction
— 80% of vagus nerve fibers send messages from body to brain — so healing is bottom-up, not just mental
— Dysfunction can be caused by stress, trauma, gut issues, infections, toxins, or poor breathing
— Doctors rarely mention it because it’s not easily tested or treated with drugs
— Signs include digestive issues, shallow breathing, wired-and-tired cycles, numbness, and emotional swings
— You can support vagus nerve health with breathwork, cold exposure, humming, movement, and safe connection
— Healing takes consistency, not hacks — but it’s possible, even without a diagnosis
— Your symptoms aren’t random — they’re your nervous system asking for safety
— Learn to listen, and the whole body starts to heal
Disclosure: The information provided is for educational purposes only and not intended as medical advice. Consult a healthcare professional before making any changes to your health routine. If you make a purchase through the links provided, I may earn a small commission at no additional cost to you.
What Is the Vagus Nerve—And Why It Matters More Than You Think?
If you’ve ever felt anxious in your gut before your brain caught up, or noticed your heart racing when you weren’t even “thinking” stressful thoughts—there’s a reason. It’s not random. It’s not just stress. It’s communication. And most of it is being carried through one, often-ignored nerve: your vagus nerve.
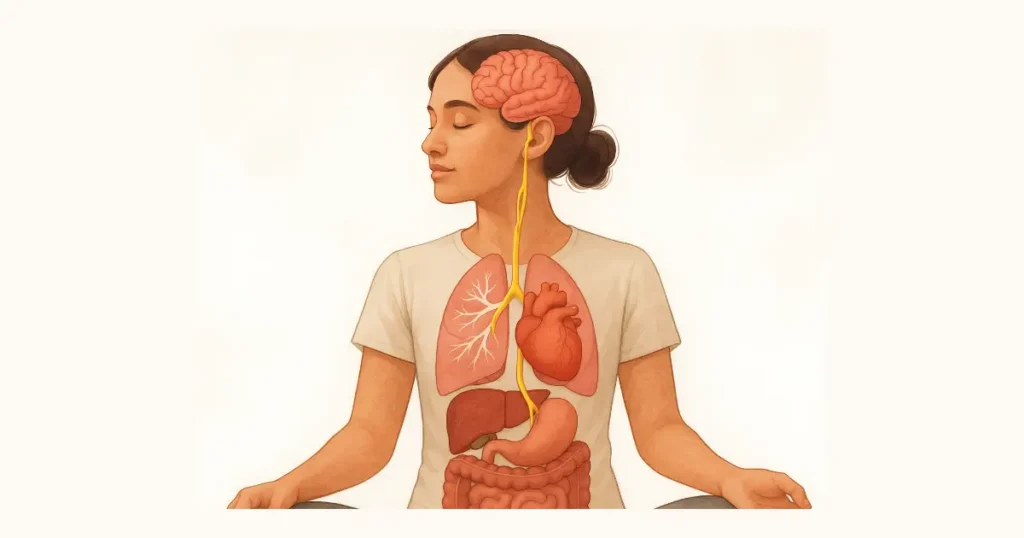
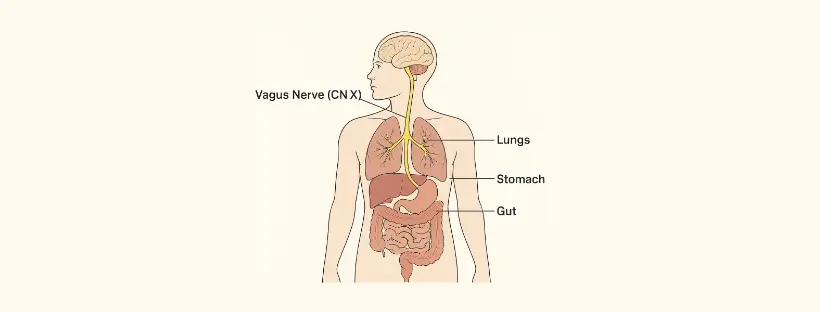
The vagus nerve (Latin for “wandering”) is the longest and most complex nerve in the body. It starts in your brainstem and travels down both sides of your neck, branching into your lungs, heart, diaphragm, stomach, intestines, liver, and more. It’s essentially the body’s information superhighway—carrying messages between your brain and your major organs.
What makes it so important is that it’s the main driver of your parasympathetic nervous system—the system responsible for “rest, digest, and repair.” When the vagus nerve is working well, it helps you feel calm, grounded, and physically safe. When it’s not, your body shifts into survival mode—keeping you wired, tired, inflamed, and often misunderstood.
Most people have no idea that the vagus nerve is quietly regulating things like:
- Heart rate and breathing
- Stomach acid, bile, and enzyme release
- Gut movement and digestion
- Inflammation control
- Immune system activity
- Neurotransmitter signaling and balance (like serotonin, dopamine, and GABA)
- Facial expression, voice tone, social connection
- Swallowing, pupil size, and even tear production
Here’s the catch: 80% of the vagus nerve’s fibers are sensory, meaning they send messages from your body up to your brain—not the other way around. That means your nervous system is constantly scanning for signals of safety or threat—and responding before you even have time to think about it. This is why physical symptoms like nausea, tight chest, or gut discomfort often show up before anxiety even has a name.
When vagus nerve signaling breaks down—due to trauma, chronic stress, inflammation, infection, or even poor sleep—it doesn’t show up on a typical test. Instead, people are often diagnosed with anxiety, IBS, panic disorder, POTS, fibromyalgia, chronic fatigue, or autoimmune symptoms. You’re sent from specialist to specialist while your core regulatory system stays ignored.
Polyvagal theory, introduced by Dr. Stephen Porges, helps explain this deeper layer. It describes two branches of the vagus nerve:
- Ventral vagus: supports calm, digestion, connection, and healing
- Dorsal vagus: shuts the system down when it feels overwhelmed or unsafe
If your body doesn’t feel safe enough for long enough, the vagus nerve can become suppressed or dysregulated—leading to either constant overdrive (anxiety, racing thoughts, palpitations) or collapse (fatigue, fog, depression, digestive shutdown). Most people oscillate between both without realizing it’s coming from the same system. Collapse isn’t weakness. It’s a survival reflex—your body’s last-ditch attempt to protect you.
This is not fringe science. It’s measurable and backed by decades of research. For example:
- Low vagal tone (a measure of how well your vagus nerve is functioning) is linked to poor stress recovery, inflammation, and emotional dysregulation (Thayer et al., 2009)
- Vagus nerve signaling from the gut plays a key role in mood and anxiety (Breit et al., 2018)
- Vagus nerve stimulation (VNS) has been shown to reduce symptoms in treatment-resistant depression, epilepsy, PTSD, and inflammatory bowel conditions (Bonaz et al., 2016; Carreno & Frazer, 2017)
- Heart rate variability (HRV)—a proxy for vagus nerve function—is now considered a critical marker for overall health and resilience (Laborde et al., 2017)
Most people have never been told this. But understanding how this one nerve works—and how to support it—can change how you see your symptoms. You don’t need to treat your digestion, mood, energy, and immunity as separate problems when they’re often being governed by the same system.
What Happens When the Vagus Nerve Breaks Down—And Why Doctors Miss It
You go to the doctor for stomach pain. Or maybe it’s your racing heart. Or the anxiety that won’t let up. You leave with a label—IBS, anxiety disorder, or just “stress.” Labs come back normal. You’re sent home with supplements, a mindfulness app, or an antidepressant.
But the symptoms persist. Nothing quite adds up.
What’s often missing is the mechanism tying it all together: a dysregulated vagus nerve.
When vagus signaling weakens, the body can’t downshift out of stress mode. Because this one nerve connects the brainstem to nearly every major organ—your gut, lungs, heart, immune system—its dysfunction rarely shows up as one clear illness. Instead, it mimics ten.
Common vagus nerve dysfunction symptoms include:
- Slow or erratic digestion (bloating, constipation, nausea)
- Racing heart or palpitations without exertion
- Shallow breathing or frequent sighing
- Brain fog, fatigue, and poor memory
- Anxiety or emotional numbness
- Low-grade inflammation and immune issues
- Sleep becomes shallow. You wake up wired, but can’t think straight. You don’t need more melatonin—you need to feel safe.
One week it feels like burnout. The next, autoimmune flares. Your system never fully resets. This happens because your body no longer receives consistent “safety” signals—and without those, it defaults to survival mode.
In more advanced cases, this breakdown in autonomic regulation can lead to diagnoses like POTS (Postural Orthostatic Tachycardia Syndrome)—a form of dysautonomia marked by dizziness, rapid heart rate, and fatigue after standing. It’s increasingly common, but Rarely discussed in terms of underlying autonomic regulation, including vagal pathways.
What makes this harder to diagnose is that vagus nerve dysfunction doesn’t show up on standard labs or imaging. Even heart rate variability (HRV)—a well-supported proxy for vagal tone—is rarely measured in conventional care. So symptoms get split up: GI issues go to gastroenterologist, chest tightness to cardiology, mood swings to psychiatry. But no one asks whether all of it could stem from a single point of dysregulation.
Research has linked low vagal tone to emotional instability, immune dysfunction, and slower recovery from stress. But most patients never hear the words vagal tone mentioned at all.
The real problem? No one’s connecting the dots.
The good news is that dysregulation isn’t permanent. But before you can repair it, you have to recognise it. These symptoms are not random. They’re your body’s early warning system—and the vagus nerve is the wire.
What Causes Vagus Nerve Dysfunction?

Vagus nerve dysfunction doesn’t happen overnight. Dysregulation usually builds over time—layer by layer—until the body can no longer return to baseline. By the time symptoms appear, the root cause has often been simmering for years.
The vagus nerve doesn’t malfunction in isolation. It becomes impaired when the system it belongs to—the autonomic nervous system—loses its capacity to self-regulate. And that can be triggered by multiple forms of stress: physical, emotional, metabolic, environmental.
Here are the most common drivers behind vagus nerve dysfunction:
- Chronic stress
Long-term activation of the stress response (HPA axis) keeps the body in fight-or-flight, suppressing parasympathetic function. Over time, vagal tone decreases, and the ability to “downshift” out of high alert is lost. - Unresolved trauma
Adverse childhood experiences (ACEs), relational trauma, or shock trauma create ongoing patterns of nervous system threat. This shapes how the vagus nerve develops and responds to the world—often toward freeze, collapse, or dissociation. - Inflammation and gut dysfunction
When the gut lining is compromised (via leaky gut, SIBO, dysbiosis, or chronic infections), it sends continuous inflammatory signals to the brain via the vagus nerve. Eventually, the nerve’s signaling becomes impaired or blunted. This is why gut health doesn’t just affect digestion—it directly shapes mood, anxiety, and nervous system stability - Viral and stealth infections
Certain viruses—especially Epstein-Barr (EBV), herpes viruses, and Lyme-related pathogens—can directly affect vagal pathways or inflame surrounding structures (like the brainstem or gut), disrupting regulation. - Toxin exposure
Mold toxins, heavy metals, and certain chemicals can impair mitochondrial energy, alter neurotransmitter function, and inflame vagus-involved pathways—especially in sensitive individuals. - Blood sugar instability
Frequent spikes and crashes in glucose dysregulate energy availability, mood, and stress response—all of which reduce vagal flexibility. - Disordered breathing
Mouth breathing, poor posture, and sleep apnea can reduce vagus nerve stimulation via the diaphragm and phrenic nerve, further impairing rest-and-digest function. - Lack of social connection or safety
From a Polyvagal perspective, humans need cues of safety—facial expressions, vocal tone, eye contact—to regulate. Chronic loneliness, unsafe relationships, or isolation deprive the vagus nerve of these inputs, reinforcing shutdown.
Dysregulation often isn’t caused by one thing—it’s cumulative. A bit of stress. A viral infection. A traumatic event. A period of poor sleep or overwork. The system gets overloaded. Neuroinflammation builds quietly in the background. The vagus nerve, responsible for switching off the alarm, starts to lose its grip. And what should have been a temporary state becomes a chronic baseline.
The body stops healing. Digestion slows. Inflammation rises. Mood fluctuates. But since no single lab can detect this process, it continues unrecognized.
That’s why symptoms like gut issues, anxiety, fatigue, or brain fog aren’t random. They’re the nervous system waving a red flag—asking for regulation that never comes.
How to Recognize Vagus Nerve Dysfunction—Even When Doctors Don’t

You won’t find “vagus nerve dysfunction” as a formal diagnosis in your chart. It’s not something your GP is testing for. There’s no single scan or lab that confirms it. But that doesn’t mean it’s not real—or that you can’t identify it.
Because here’s the truth:
When the vagus nerve stops doing its job, everything else starts falling apart.
You just haven’t been taught to trace the pattern.
This nerve controls the very systems that keep you stable: digestion, heart rate, inflammation, immunity, breathing, emotional regulation. If it becomes dysregulated, your body starts sounding the alarm—but instead of seeing the full picture, most people (and most doctors) treat the fallout symptom by symptom.
So how do you know if the vagus nerve is involved?
Start by looking for the pattern—not just isolated issues, but how they cluster.
Signs of a potentially dysregulated vagus nerve:
- You swing between anxiety and exhaustion, wired then wiped out
- Your gut reacts to stress (constipation, bloating, nausea, IBS diagnosis)
- You experience palpitations, chest tightness, or shallow breathing—even at rest
- You feel detached, numb, or “checked out” for no clear reason
- You’ve had chronic inflammation, autoimmune symptoms, or poor immune response
- You’ve been told your symptoms are “just stress”—but they never fully go away
- You’ve tried all the right things (supplements, diets, meds) but still don’t feel well
If more than a few of these feel familiar, you’re not broken. You’re dysregulated.
And the common denominator is often your vagus nerve.
Why It Gets Missed
Vagal dysfunction doesn’t look the same in everyone.
It mimics other conditions—anxiety, depression, POTS, long COVID, fibromyalgia, SIBO, even panic disorder. And because it doesn’t show up on standard bloodwork or imaging, it’s rarely flagged.
Even HRV (heart rate variability), the most studied marker of vagus nerve activity, isn’t something most doctors track unless they’re in cardiology or elite sports medicine.
And this is where most people give up:
No diagnosis, no help.
But you don’t need a diagnosis to start healing.
What you need is awareness—and a willingness to stop chasing disconnected symptoms and start supporting the system that governs them all.
This isn’t about self-diagnosing. It’s about reconnecting with the part of your body that’s been left out of the conversation—and learning what it’s been trying to tell you all along.
How to Support Vagus Nerve Function Naturally

You can’t supplement your way out of a dysregulated nervous system. And you can’t deep-breathe your way out of chronic inflammation. But you can start by giving your system a new signal. Even one honest exhale can begin to shift your state. Once your body gets a taste of safety, it remembers the way back.
This isn’t about hacking your body. It’s about restoring function.
The vagus nerve is a sensory pathway—it listens more than it talks. That means most of its regulation happens from the bottom up (body to brain), not just top-down (thoughts to body). So while mindset matters, real healing starts with physiology.
Daily practices that improve vagal tone:
- Diaphragmatic breathing
Slow, deep breaths through the nose—especially with a longer exhale—stimulate vagus nerve endings near the diaphragm. Aim for 4–6 breaths per minute to shift into parasympathetic mode. - Cold exposure
Brief cold water immersion (face splashes, showers, or baths) activates the vagus nerve via the mammalian dive reflex, helping reduce inflammation and improve stress tolerance. - Gargling, humming, or singing
The vagus nerve innervates muscles at the back of the throat and vocal cords. These mechanical vibrations send stimulation back up the vagal pathway. - Movement with rhythm
Walking, dancing, rocking, or any repetitive motion engages vagus nerve circuitry—especially when paired with calm breathing. - Safe social connection
Eye contact, tone of voice, and feeling “seen” by another person directly engage the ventral vagus system—your body’s built-in safety circuit. - Grounding nutrition
Nutrient-dense, anti-inflammatory meals support gut function (which feeds the vagus nerve), while blood sugar stability protects nervous system balance. Avoid ultra-processed foods, seed oils, and artificial sweeteners—all known to impair gut-brain signaling.
The vagus nerve can be retrained. But it needs consistency. You can’t reset a nervous system that doesn’t feel safe, or heal a gut that’s under constant stress. Start with one or two practices that signal to your body: “You’re okay now. We’re not in danger anymore.”
It’s not a quick fix. But it’s a lasting shift.
Why Your Doctor May Not Mention the Vagus Nerve

If the vagus nerve matters so much, why hasn’t your doctor brought it up?
Simple: because the system they were trained in wasn’t designed to look for it.
Medical school teaches doctors how to diagnose disease and prescribe treatment. If it doesn’t show up on a scan or respond to a drug, it often gets ignored. That includes the vagus nerve—even though it regulates digestion, heart rate, immunity, mood, and inflammation.
Most people never learn that the body runs on one unifying system—your nervous system. Instead, they’re sent to a GI for their gut, a cardiologist for their heart, and a psychiatrist for their mood, while the real root issue goes undiagnosed.
Why? Because you can’t sell the nervous system.
You can’t patent breathwork or trauma repair. You can’t make billions from fiber, sunlight, or polyvagal theory. But you can build industries around managing anxiety, IBS, insomnia, and chronic inflammation—separately.
That’s what the modern healthcare model rewards: treating symptoms in parts, not seeing the pattern.
Doctors aren’t ignoring the vagus nerve on purpose. But most medical education is funded or influenced by pharmaceutical and device industries. That shapes what gets taught, tested, and trusted:
- A 2002 JAMA study found 87% of clinical guideline authors had financial ties to drug companies.
- A 2013 PLOS Medicine review showed disease definitions were often expanded by panels with industry ties.
- Continuing medical education (CME)—required for licensed doctors—is still largely backed by pharma.
Even textbooks aren’t immune. When the system is built around selling solutions, the nervous system gets left out—because it doesn’t sell.
And here’s the deeper problem: many medications manage symptoms without addressing upstream regulation. They manage downstream symptoms (like gut issues, mood swings, or insomnia) without addressing upstream dysfunction, like poor vagus nerve signaling.
If a doctor recommends non-drug interventions—even with evidence—they risk stepping outside their clinical “standard of care.” Which is why most don’t. Not because you don’t deserve the truth. But because they’re bound to a system that profits from keeping the body fragmented.
It’s not that the science isn’t there.
It’s that the system isn’t built to teach it.
And until that changes, the vagus nerve will stay invisible—while the symptoms it causes are treated in silos.
Final Thoughts: Why the Vagus Nerve Deserves Your Attention

If you’ve been chasing symptoms across your gut, heart, mood, energy, and immune system—and finding no clear answers—it’s not in your head. It’s in your wiring.
The vagus nerve isn’t a fringe wellness concept. It’s the master regulator of how your body returns to safety, and when it’s out of sync, nothing works like it should.
Most doctors won’t mention it. Not because they don’t care, but because the system they were trained in isn’t designed to connect these dots. It’s designed to manage symptoms, not ask why they’re happening.
But that doesn’t mean you’re stuck.
Understanding how the vagus nerve works—and how to support it—can turn frustration into clarity. It doesn’t require a diagnosis. It doesn’t require perfection. It just starts with noticing the signals, and choosing to respond differently.
Your body isn’t broken. It’s been trying to get your attention.
Now you know how to listen.